This post is part of a series on gluten and its various reactions. In this post I’ve asked Dr. Fasano and his team to break down the markers for Celiac Disease so you can clearly discuss testing with your own doctor. Many thanks to Dr. Fasano and his team (especially Susie) for helping me put this together.
Background: No One Can Digest Gluten
During Part 1 of my interview with Alessio Fasano, M.D. of the University of Maryland’s Celiac Research Center, we have learned that no one can properly digest gluten, or more specifically, "gliadin", a protein found in wheat. This blew me away.
We simply don’t have it in us -- the enzyme(s), that is. According to Dr. Fasano, our bodies haven’t yet evolved the ability to process this fairly modern grain called "wheat". Modern science has also increased the protein content of wheat by 14% in recent years. In terms of human digestion, that's a big deal. You see, our bodies need specific enzymes to break down gliadin from its amino acid form (of glutamine and proline) into elements small enough for us to digest. Humans don’t have these enzymes. The enzymes that we do have can only break down gliadin into peptides -- elements too large for our small intestines to absorb. So in an effort to gather nutrients; our small intestines separate to let the peptides through. As Dr. Fasano put it, “the gliadin cross-talks with our cells, confusing them and causes our small intestines to leak.”
In a “normal” person, the intestinal walls still separate improperly, but the peptide passes through the digestive tract unnoticed by their immune system. When someone has a reaction (such as gluten sensitivity or an allergy), that person’s immune system recognizes the larger peptide as an enemy (its not supposed to be there) and rushes to protect. If that person has celiac disease, the immune system gets so confused that it turns on the intestinal walls themselves, damaging them. The gluten is the "trigger" for this autoimmune disease. And celiac disease is the only auto-immune disease with a clear trigger.
The only treatment of celiac disease, or any immune reaction to gluten, is to completely remove all wheat (and also similar protein-containing rye, barley, spelt and triticale) from your diet. Some people also need to remove oats.
THERE ARE 3 FORMS OF GLUTEN-BASED REACTIONS: Celiac Disease, Gluten Sensitivity, and a Gluten/Wheat Allergy. There are four different types of wheat allergy -- and each type behaves differently.
Note: Gluten Sensitivity has many of the same symptoms. In Part 3 we will address some frequently asked questions about Gluten Sensitivity.
In this post I’ve asked Dr. Fasano and his team to break down the markers for Celiac Disease so you can clearly discuss testing with your own doctor.
Markers for Celiac Disease Testing
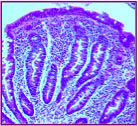
 Biopsy showing normal intestinal villi, or "Stage 0". (Used with permission of The Center for Celiac Research) According to Dr. Fasano in our interview, the latest research shows that you could have 4 out of the first 5 of the following markers in order to be diagnosed with Celiac Disease. If your doctor finds that you have 4 markers before your biopsy, you may be able to avoid doing the biopsy, however, the biopsy is the gold diagnostic standard* (this is no longer considered to be true, please see 2014 update below).
Biopsy showing normal intestinal villi, or "Stage 0". (Used with permission of The Center for Celiac Research) According to Dr. Fasano in our interview, the latest research shows that you could have 4 out of the first 5 of the following markers in order to be diagnosed with Celiac Disease. If your doctor finds that you have 4 markers before your biopsy, you may be able to avoid doing the biopsy, however, the biopsy is the gold diagnostic standard* (this is no longer considered to be true, please see 2014 update below).
*UPDATE: In my 2014 interview with Dr. Fasano, he updates this information and says that the biopsy is no longer the gold standard for celiac diagnosis. It is an important marker, but only after the other 4 out of 5 markers warrant it.
Read the 2014 interview & the updated information here.
Marker #1: Symptoms
Symptoms of celiac disease include diarrhea, constipation, weight loss, abdominal pain, chronic fatigue, weakness, malnutrition, and other gastrointestinal problems. In children, the symptoms may include failure to thrive (an inability to grow and put on weight), irritability, an inability to concentrate, diarrhea and bloating. Further, people affected by celiac disease may experience extra-intestinal symptoms that involve many systems and organs including bones (osteoporosis, arthritis, and joint pain), blood (anemia and bleeding), reproductive system (infertility and reoccurring abortion), nervous system (chronic fatigue syndrome, depression, dementia), and behavioral changes.
Note: Another manifestation of celiac disease is a skin rash called "Dermatitis Herpetiformis" (DH). A skin biopsy is typically taken to determine if you have this manifestation.
Marker #2: A positive blood test
 Biopsy Showing Stage 1: Infiltrative Damage to the mucosal lining of the small intestine. (Used with permission of The Center for Celiac Research)There is a particular series of blood tests called the ‘Celiac Panel'". These tests measure your immune system’s response to gluten in the food you eat.
Biopsy Showing Stage 1: Infiltrative Damage to the mucosal lining of the small intestine. (Used with permission of The Center for Celiac Research)There is a particular series of blood tests called the ‘Celiac Panel'". These tests measure your immune system’s response to gluten in the food you eat.
- tTG-IgA or tissue transglutaminase-IgA
- AGA-IgG or Antigliadin IgG
- AGA-IgA or Antigliadin IGA
- Total IGA
The presence of tTG antibodies is highly suggestive of Celiac Disease, while AGA can be elevated also in cases of wheat allergy.
Marker #3: Genetic Compatibility
 Biopsy Showing Stage 2: Hyperplastic - the villi are shrinking and flattening. (Used with permission of The Center for Celiac Research)As an autoimmune disease, Celiac Disease is the consequence of the interplay between genes and the environment (gluten). We don’t know all the necessary genes to develop Celiac Disease; however, HLA DQ2 and/or DQ8 are absolutely necessary to develop the disease. Since one-third of the general population also has these genes, the presence of DQ2 or DQ8 does not imply that the person will develop Celiac Disease, rather, that they have a genetic compatibility with Celiac Disease. Conversely, the absence of DQ2/DQ8 almost certainly rules out Celiac Disease.
Biopsy Showing Stage 2: Hyperplastic - the villi are shrinking and flattening. (Used with permission of The Center for Celiac Research)As an autoimmune disease, Celiac Disease is the consequence of the interplay between genes and the environment (gluten). We don’t know all the necessary genes to develop Celiac Disease; however, HLA DQ2 and/or DQ8 are absolutely necessary to develop the disease. Since one-third of the general population also has these genes, the presence of DQ2 or DQ8 does not imply that the person will develop Celiac Disease, rather, that they have a genetic compatibility with Celiac Disease. Conversely, the absence of DQ2/DQ8 almost certainly rules out Celiac Disease.
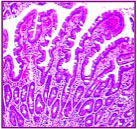
Marker #4: An Intestinal Biopsy
 Intestinal biopsy showing Stage 3a, or partial atrophy of the lining of the small intestine. (Photo used with permission from The Center for Celiac Research)A biopsy is really the gold standard for diagnosing Celiac Disease.
Intestinal biopsy showing Stage 3a, or partial atrophy of the lining of the small intestine. (Photo used with permission from The Center for Celiac Research)A biopsy is really the gold standard for diagnosing Celiac Disease.
NOTE: In my 2014 interview with Dr. Fasano, he says that the biopsy is no longer the gold standard for celiac diagnosis. It is an important marker, but only after the other 4 out of 5 markers warrant it.
Read the 2014 interview & the updated information here.
If blood tests and symptoms suggest celiac disease, a biopsy of the small intestine is usually taken to confirm that diagnosis. During the biopsy, the doctor removes tiny tissue samples from the small intestine to check for damage to the intestinal villi. To grab the sample, a doctor threads a long, thin tube called an endoscope through the patient's mouth and stomach, then into the small intestine. Using the endoscope as a tunnel, the doctor passes instruments into the small intestine in order to retrieve the sample.
A Marsh Score is used to determine how far the celiac disease has advanced. Scoring starts at "0" and ends at "4". If the mucosa (intestinal lining) is normal, celiac disease is unlikely, or "Stage 0". This is also known as the "pre-infiltrative stage." Stage 4 indicates a total flattening (or atrophy) of the villi in the small intestine. The villi allow nutrients from food to be absorbed by the small intestine. Without healthy villi, we become mal-nourished, even if we eat like a horse.
Marker #5: The symptoms resolve (go away) with a gluten-free diet.
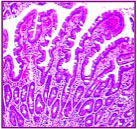
 Biopsy showing Stage 3b - subtotal atrophy of the small intestine where the villi are shrinking and flattening (Photo used wtih permission of the Center for Celiac Research)A gluten-free diet is more than simply taking bread out of your meals. Gluten can be "hidden" within ingredients like smoke flavoring or barley malt (among many others). Gluten also is in many cosmetics and beauty products. In addition, certain products that do not inherently contain gluten can be processed with wheat, such as other flours or nuts; and as a result, processed foods can have a great deal of cross contamination.
Biopsy showing Stage 3b - subtotal atrophy of the small intestine where the villi are shrinking and flattening (Photo used wtih permission of the Center for Celiac Research)A gluten-free diet is more than simply taking bread out of your meals. Gluten can be "hidden" within ingredients like smoke flavoring or barley malt (among many others). Gluten also is in many cosmetics and beauty products. In addition, certain products that do not inherently contain gluten can be processed with wheat, such as other flours or nuts; and as a result, processed foods can have a great deal of cross contamination.
NOTE: A stool sample test, which can recognize positive antibodies, is also available. But at this point stool samples are not considered as a reliable diagnostic tool by the medical community.
See: The Most Surprising Places for Hidden Gluten
Long-term Health Consequences & Treatment
Celiac disease can be life threatening. If you don't entirely remove gluten from your diet, celiac  Stage 4: Biopsy showing total atrophy of the mucosal lining. The intestinal villi are completely flattened. (Used with permission from the Center for Celiac Research)disease can have long term and serious health consequences. I stress this, because I’ve heard those newly diagnosed ask, “How much gluten can I eat?” Then some bad advice in return, “Well, it depends upon how bad your celiac disease is.” There may be degrees of damage caused by the illlness, but there is no corresponding degree of treatment. The only treatment for celiac disease is a completely gluten-free diet.
Stage 4: Biopsy showing total atrophy of the mucosal lining. The intestinal villi are completely flattened. (Used with permission from the Center for Celiac Research)disease can have long term and serious health consequences. I stress this, because I’ve heard those newly diagnosed ask, “How much gluten can I eat?” Then some bad advice in return, “Well, it depends upon how bad your celiac disease is.” There may be degrees of damage caused by the illlness, but there is no corresponding degree of treatment. The only treatment for celiac disease is a completely gluten-free diet.
Celiacs are more likely to be afflicted with problems relating to malabsorption, including osteoporosis, tooth enamel defects, central and peripheral nervous system disease, pancreatic disease, internal hemorrhaging, organ disorders (gall bladder, liver, and spleen), and gynecological disorders. Untreated celiac disease has also been linked an increased risk of certain types of cancer, especially intestinal lymphoma _Center for Celiac Research
Creative Healing
The good news is, that if you do remove gluten from your diet, and your diagnosis is celiac disease, your health can and probably will improve. Your intestines can return to normal, and your risk for other diseases greatly reduced.
The villi are not permanently damaged. The intestine is an organ, which renews itself every three days. Therefore, if the damage is exclusively due to CD, the villi will be reformed once on a gluten-free diet. The time for the villa to return to normal varies among individuals. _Center for Celiac Research
To heal, tap into your creative juices and approach eating with a different mindset. Your life now includes minimally processed whole foods and constant label reading. You will need to carefully choose restaurants and speak up to your friends, family and hosts, whomever they may be. Don't eat anything unless you know exactly what it contains. If you are recently diagnosed, become an information junkie about your disease and learn, learn, learn. The Tender Palate (The Tender Foodie), The Center for Celiac Research and other great resources are here to help. With some changes, a healthy, satisfying life is just around the corner.
Other Articles on Gluten-based Reactions
PART ONE: Interview w/ Dr. Alessio Fasano: Should Anyone Eat Gluten?
PART THREE: Gluten Sensitivity - A New Food Allergy
For More information, The University of Maryland Center for Celiac Research has a wealth of videos, articles and FAQs to help guide you.
About Dr. Fasano & the Center For Celiac Research
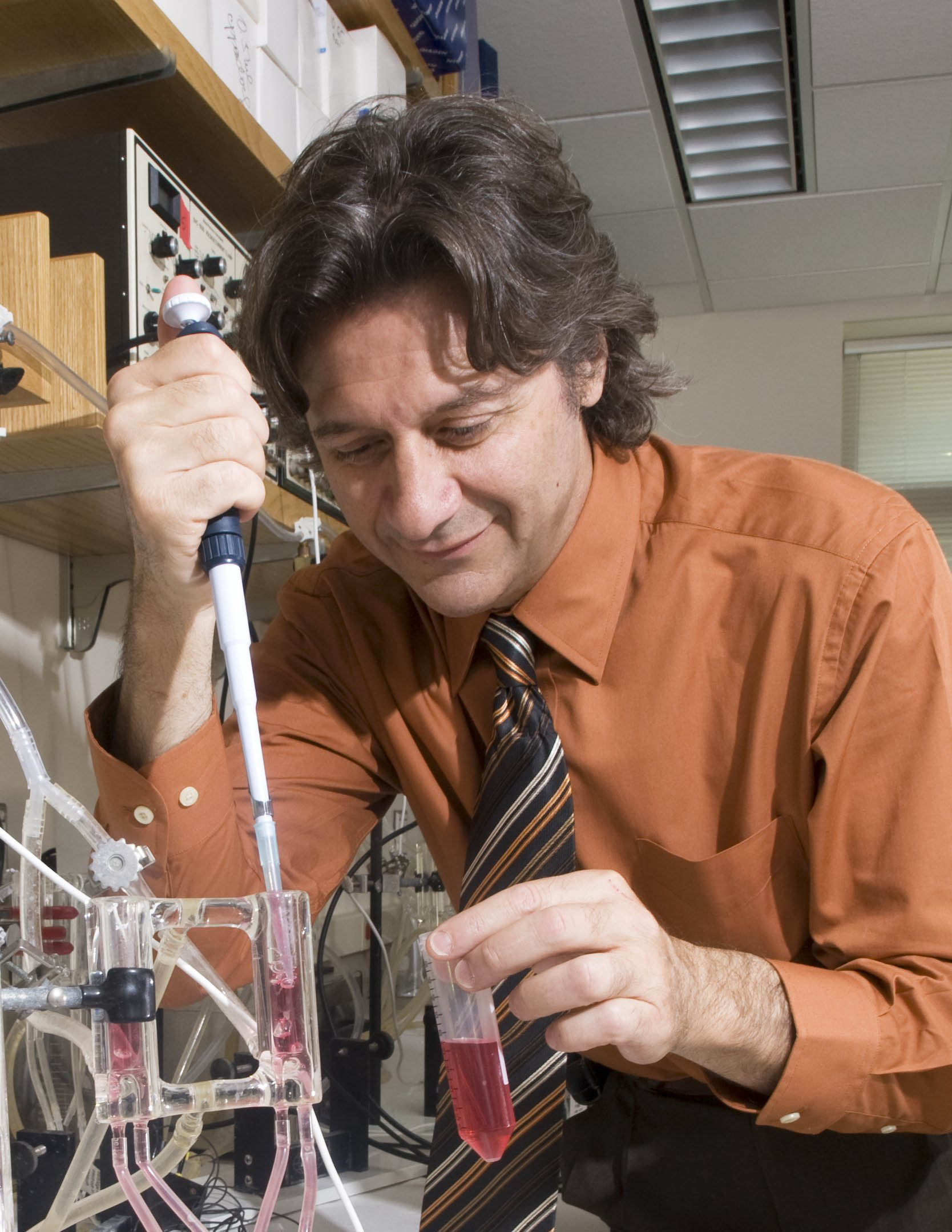 Alessio Fasano, M.D., is the director of the University of Maryland Center for Celiac Research, professor of pediatrics, medicine and physiology at the University of Maryland School of Medicine and director of the Mucosal Biology Research Center at the University of Maryland School of Medicine. Dr. Fasano is an expert on gluten/wheat allergies and celiac disease. In 2011, he led the research team who discovered a new immune reaction called "gluten sensitivity".
Alessio Fasano, M.D., is the director of the University of Maryland Center for Celiac Research, professor of pediatrics, medicine and physiology at the University of Maryland School of Medicine and director of the Mucosal Biology Research Center at the University of Maryland School of Medicine. Dr. Fasano is an expert on gluten/wheat allergies and celiac disease. In 2011, he led the research team who discovered a new immune reaction called "gluten sensitivity".
University of Maryland Center for Celiac Research is an institution engaged in clinical care, diagnostic support, education, and clinical and basic science research in Celiac Disease.
The paramount goal of the Center for Celiac Research is to increase the awareness of Celiac Disease in order to provide better care, better quality of life, and more adequate support for the Celiac Disease community. To view the CFCR's brochure, CLICK HERE.
 Thursday, May 24, 2012 at 7:13PM
Thursday, May 24, 2012 at 7:13PM  Melanie Potock, MA, CCC-SLP tagged
Melanie Potock, MA, CCC-SLP tagged  behavioral treatment,
behavioral treatment,  biopsy,
biopsy,  celiac disease,
celiac disease,  endoscopy,
endoscopy,  gluten,
gluten,  gluten sensitivity
gluten sensitivity  Email Article
Email Article  Print Article in
Print Article in  Health,
Health,  Parents/Kids
Parents/Kids 
 Melanie Potock, MA, CCC-SLPMelanie is speech language pathologist who specializes in feeding. Her work brings her into the homes and schools of her clients, kids, who for various reasons have difficulty with food or with eating. She works with kids and their parents to develop effective strategies that help children become “more adventurous eaters”. At least 50% of her clients have food allergies or intolerances, and for them, “adventurous eating” takes on a special meaning. Melanie is also the author of Happy Mealtimes with Happy Kids” and the executive producer of “Dancing in the Kitchen.”
Melanie Potock, MA, CCC-SLPMelanie is speech language pathologist who specializes in feeding. Her work brings her into the homes and schools of her clients, kids, who for various reasons have difficulty with food or with eating. She works with kids and their parents to develop effective strategies that help children become “more adventurous eaters”. At least 50% of her clients have food allergies or intolerances, and for them, “adventurous eating” takes on a special meaning. Melanie is also the author of Happy Mealtimes with Happy Kids” and the executive producer of “Dancing in the Kitchen.”