Interview w/ Dr. Alessio Fasano, Part 1: Should Anyone Eat Gluten?
 Monday, December 19, 2011 at 1:23PM
Monday, December 19, 2011 at 1:23PM  Elisabeth Veltman, The Tender Foodie tagged
Elisabeth Veltman, The Tender Foodie tagged  celiac disease,
celiac disease,  doctor visits,
doctor visits,  food allergies,
food allergies,  gluten,
gluten,  new research,
new research,  research,
research,  sensitivity,
sensitivity,  wheat allergies
wheat allergies  Email Article
Email Article  Print Article in
Print Article in  Doctor Visits,
Doctor Visits,  Food Allergy Facts,
Food Allergy Facts,  Research
Research
 Alessio Fasano, M.D., Medical Director for the Center for Celiac ResearchSince March of this year (2011), I’ve had it on my list to speak to Alessio Fasano, the Medical Director for The University of Maryland’s Center for Celiac Research. What happened in March? Honest-to-goodness food allergy research happened, that’s what. Scientists now have a better understanding of why it seems like everyone (and his or her brother) “suddenly” has trouble eating wheat, rye, and barley.
Alessio Fasano, M.D., Medical Director for the Center for Celiac ResearchSince March of this year (2011), I’ve had it on my list to speak to Alessio Fasano, the Medical Director for The University of Maryland’s Center for Celiac Research. What happened in March? Honest-to-goodness food allergy research happened, that’s what. Scientists now have a better understanding of why it seems like everyone (and his or her brother) “suddenly” has trouble eating wheat, rye, and barley.
Ten years ago, most of us didn’t know what it was. But now “gluten” is a household buzzword. Even if we don’t understand what “gluten” actually means (or even is), we see menus and products that are free of it. I would also wager that every person in the U.S. knows someone who gets sick after eating it.
Quick Facts
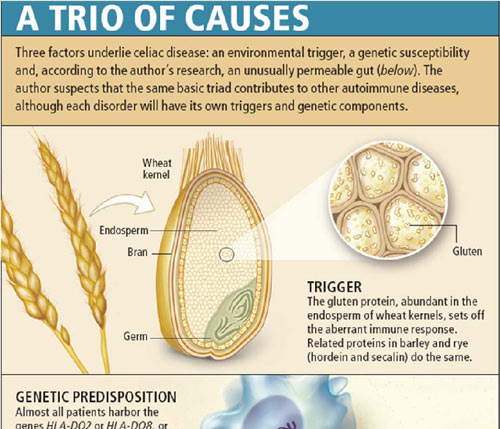
Gluten is that pesky protein that is unusually rich in the amino acids glutamine and proline. The gluten protein (really, the "gliadin" protein) is found in wheat, with similar trouble-causing proteins found in rye, barley, and triticale.
Because of studies that people like Dr. Fasano and his team have done, we know things we didn’t know before. Things like:
- There are four different kinds of wheat allergies, with four different types of immune responses.
- We also now know that 18 million people (aka everyone and his/her brother) have a newly discovered immune response called “gluten sensitivity.” People with this condition can have up to 100 symptoms, many similar to Celiac Disease. The difference is that Gluten Sensitivity does not involve the immune system attacking the intestinal wall of the patient.
- The number of people with Celiac Disease has quadrupled in the last 50 years.
- Once thought a genetic disease triggered in childhood, recent cases of celiac disease have shown up in people who are in their 70’s and in people who have genetic markers but no genetic history of the disease.
- Celiac Disease is the only autoimmune disease that has a clear trigger (gluten). Therefore, scientists may be able to learn how to better manage other autoimmune diseases, like diabetes, multiple sclerosis, and rheumatoid arthritis through research on celiac disease.
- Today, 1 in 133 people have celiac disease, a genetically linked, autoimmune response to gluten. That’s more than 2 million people in the U.S., and 1 percent of the global population. However, most do not know it.
The Interview
I was most privileged to speak with Dr. Fasano about gluten, our bodies’ response(s) to it, allergies, Celiac Disease, and what Dr. Fasano calls “the new kid on the block,” Gluten Sensitivity. We discussed why there are so many issues with gluten and how you can get tested for an immune reaction to it.
I learned a great deal from Dr. Fasano, including the fact that no one can digest gluten. I know, this surprised me, too; so I asked again and got the same answer. No one can digest gluten. Not properly.
Read on, oh seekers of answers.
TF: Why did you do this most recent study on gluten?
It started about two or three years ago after a critical mass of people with various symptoms came to our clinic, and the numbers of these particular people increased exponentially at that time. Though they had symptoms similar to Celiac Disease, they did not have Celiac Disease. We would give them a negative diagnosis for celiac disease, but they kept coming back with the same symptoms. Many had started a gluten-free diet on their own, and the gluten-free diet seemed to be a cure, a miracle. We had reached the conclusion that though this group of people did not have Celiac Disease, there must be something else happening that is gluten related.
TF: I understand that there was some research to build upon, correct? Tell me about the Banana Babies Study. How did Celiac & Gluten Sensitivity research all begin?
Shortly after World W Untreated children with Celiac Disease. Photo used with permission from the UMD Center for Celiac Researchar II, we learned that gluten was the cause for the onset of Celiac Disease, thanks to the Dutch pediatrician, Willem-Karel Dicke. He was puzzled by high infant mortality rates (due to unknown celiac disease) after the war, because in the last few years of the war when bread was unavailable, the mortality rate (from this condition) was 0.. Dicke noticed that these kids improved without bread, and that their condition deteriorated when bread became available again.
Untreated children with Celiac Disease. Photo used with permission from the UMD Center for Celiac Researchar II, we learned that gluten was the cause for the onset of Celiac Disease, thanks to the Dutch pediatrician, Willem-Karel Dicke. He was puzzled by high infant mortality rates (due to unknown celiac disease) after the war, because in the last few years of the war when bread was unavailable, the mortality rate (from this condition) was 0.. Dicke noticed that these kids improved without bread, and that their condition deteriorated when bread became available again.
The modern era of gluten research started, however, with Samuel Ghee in the United Kingdom at the end of the 19th Century. He gave a famous speech (in a lecture at the Hospital for Sick Children, Great Ormond Street in 1887) based on his report called, “On the Coeliac Affection.” Ghee knew what Celiac Disease was (a chronic, genetically pre-disposed, digestive disease that can affect any age), knew that diet was involved, but didn’t know what triggered it. It is believed that he also followed the observations of a physician named Aretaeus the Cappadocian, who with others had described the celiac state more than 2000 years before his time.
 1st Case of Celiac Disease at U of Maryland in 1938 being treated. Photo used with permission from The Center for Celiac Research.
1st Case of Celiac Disease at U of Maryland in 1938 being treated. Photo used with permission from The Center for Celiac Research.
Before Dicke's discovery and development of the gluten-free diet, one of the diets physicians tried with the afflicted children was the banana diet, used at the University of Maryland in the 1930s. Bananas contain enough calories and nutrients for survival. Parents were instructed to drop their children off for 6 months, and if they were still alive, they could pick them up and take them home.
TF: Did any Banana Babies survive?
Oh yes, in fact there are some survivors who are still around! In fact I invited a Banana Baby who was treated at the University of Maryland Hospital in the 1930s, Barbara Hudson, to speak during one of my recent lectures. She is doing great!
Listen to Dr. Fasano and Barbara Hudson Speak
TF: How many forms of gluten reactions are there?
Dr. Fasano: There are 3 forms. Celiac Disease, and Gluten Sensitivity, and Gluten/Wheat Allergy – and there are four different types of wheat allergy that all behave differently.
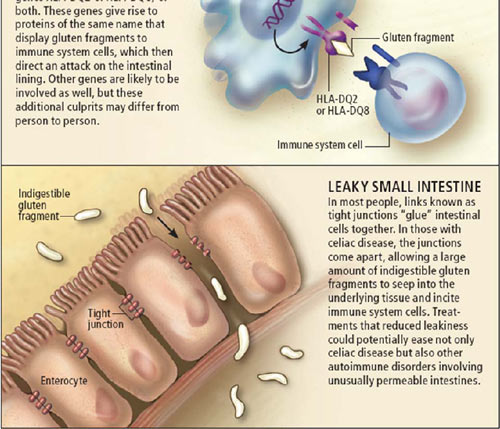
TF: What is behind all of these reactions?
Dr Fasano: Gliadin. Gliadin is one of the proteins found in gluten. When someone has a reaction, it’s because gliadin cross talks with our cells, causes confusion, and as a result, causes the small intestine to leak. Gliadin is a strange protein that our enzymes can’t break down from the amino acids (glutamine and proline) into elements small enough for us to digest. Our enzymes can only break down the gliadin into peptides. Peptides are too large to be absorbed properly through the small intestine. Our intestinal walls or gates, then, have to separate in order to let the larger peptide through. The immune system sees the peptide as an enemy and begins to attack. The difference is that in a normal person, the intestinal walls close back up, the small intestine becomes normal again, and the peptides remain in the intestinal tract and are simply excreted before the immune system notices them. In a person who reacts to gluten, , the walls stay open as long as you are consuming gluten. How your body reacts (with a gluten sensitivity, wheat allergy or Celiac Disease) depends upon how long the gates stay open, the number of “enemies” let through and the number of soldiers that our immune system sends to defend our bodies. For someone with Celiac Disease, the soldiers get confused and start shooting at the intestinal walls.
 Used with permission from the Center for Celiac Research
Used with permission from the Center for Celiac Research
TF: That sounds like everyone is gluten intolerant in some way. Is that true? Everyone?
Yes. No one can properly digest gluten. We do not have the enzymes to break it down. It all depends upon how well our intestinal walls close after we ingest it and how our immune system reacts to it.
TF: Why have so many people been diagnosed within the last few years?
Dr. Fasano: Some of this is because the medical community has become more aware and because there has been an increase in the incidents (of gluten reactions) in recent years. The environment in general is also a factor. The quantity of grains that we now eat has increased. Breast-fed babies seem to be more protected from developing adverse reactions to gluten. We’ve found that certain good bacteria, or probiotics that live within us also play a part in “turning off” an adverse reaction to gluten. Antibacterial soaps and other things are reducing the number of these bacteria, changing the microbial environment in our gut.
TF: You’ve mentioned in the study that Agricultural Changes in Wheat have played a role. Can you tell me more about this?
Dr. Fasano: Ten thousand years ago there were no gluten grains. Wheat, rye, barley and triticale are relatively new grains that have been introduced to our diet. We haven’t had enough time to evolve in order to digest these grains properly. In recent years the protein content has increased greatly in our modern wheat. Now, 14% of dry wheat is gluten. This is a lot. I understand why this has happened - more gluten gives characteristics to baked goods that are more desirable, like more elasticity; it’s more palatable, but less digestible.
TF: What about GMO’s (Genetically Modified Organisms)?
Dr. Fasano: These are all GMOs’! (Dr. Fasano indicated that we’ve been manipulating agriculture for a long time*). The problem is that if you do this too fast, like we’ve done in the last 50 years, we pay a price. It takes centuries for our bodies to adapt. There is always a balance between the advantages and the disadvantages. Agricultural mutations are all by chance so it takes time to rule out problems that are created by these mutations. It is unfair to blame GMOs as the only cause, although they are a factor. Our immune system evolved to only fight one enemy, bacteria. Now we have a host of environmental toxicities to fight and each person’s immune system does its best to manage those.
(*Note: It's important to note that we did not discuss the types of genetically modified mutations, such as seeds created to withstand pesticides or those that actually produce pesticides.)
TF: Are certain countries more prone to have a population with gluten sensitivity, gluten allergies or Celiac Disease?
Dr. Fasano: In earlier years, Celiac Disease was more common in Ireland and Italy, so it was typically easier to diagnose. People of European descent had a higher tendency to carry the genetic code that predisposes someone to that disease. Now, with the recipe of DNA plus the availability of gluten, Celiac Disease is being found at a surprising rate in India and China. As the quality of life and income improves in these countries, their diet is changing, and it now includes gluten. So, there is a rise in Celiac Disease and in Gluten Sensitivity everywhere.
TF: You’ve mentioned earlier that doctors are diagnosing more cases. Do you feel that awareness has increased in the last 5 years?
Dr. Fasano: Oh yes. Physicians are more aware, and because of this (Gluten Sensitivity) study they have more information. But we still need to learn a lot--starting with understanding the many symptoms associated with Gluten Sensitivity and Celiac Disease. Celiac Disease is systemic (it affects a number of organs and tissues). Doctors need to better understand how to test and diagnose it. Nutritionists are the ones to help patients manage food allergies and Celiac Disease, not the doctors. Doctors, however, need to learn about this new entity called Gluten Sensitivity. We all need to be able to clearly define these conditions and speak in the same language. And that starts with the right tools to diagnose gluten-related disorders.
TF: What are the markers for Celiac Disease that doctors and patients should look for?
Dr. Fasano: The latest research shows that you could have 4 out of the first 5 of the following markers for Celiac Disease. Gluten Sensitivity has many of the same symptoms. (Please see "Part Two: How to Get Tested for Celiac Disease" for these markers and their in-depth descriptions.")
NEXT UP
PART TWO: How to Get Tested for Celiac Disease
PART THREE: Gluten Sensitivity - A New Food Allergy
For more frequently asked questions on testing for Celiac Disease and Gluten Sensitivity, visit the Center for Celiac Research’s website.
-------------------------------------------------------------------------------------------------------------------
University of Maryland Center for Celiac Research is an institution engaged in clinical care, diagnostic support, education, and clinical and basic science research in Celiac Disease.
The paramount goal of the Center for Celiac Research is to increase the awareness of Celiac Disease in order to provide better care, better quality of life, and more adequate support for the Celiac Disease community. To view the CFCR's brochure, CLICK HERE.